
Image credit: Parentdish
Having miscarriage is such a sad event for couples. Surprisingly, majority of the causes are preventable.
Recurrent miscarriage is when there is spontaneous (not voluntary) consecutive two or more termination of pregnancy before the age of viability (24 weeks in UK and 28 weeks in Nigeria). Most spontaneous loss of pregnancy happens within the first trimester (13 weeks).
Recurrent miscarriage is not a single disease entity but is a syndrome that may have one or more causes. Examples of causes include abnormally shaped uterus, uterine fibroid, previous scar on the uterus preventing implantation, hormonal imbalances e.g. prolactin, thyroid hormone, progesterone; cervical incompetence.
Cervical incompetence is the inability of the cervix to be able to carry pregnancy to term due to functional or structural abnormalities. It is the commonest cause of second trimester abortion (33%).
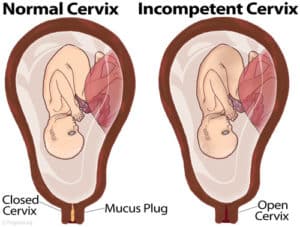
Image credit: www.pregmed.org
It is probable that cervical length and strength, together with the quality of the cervical mucus, contribute towards cervical function, both to retain the pregnancy within the uterus and to exclude potential bacterial pathogens from ascending from the vagina. Numerous studies have demonstrated a strong relationship between cervical length and the risk of recurrent miscarriage. The cervix may be damaged (or completely removed) by surgery in the treatment of cervical cancer or, rarely, during a difficult instrumental vaginal delivery, or caesarean section at full dilatation.
RISK FACTORS FOR CERVICAL INCOMPETENCE
The following risk factors can make you have cervical incompetence hence recurrent miscarriage:
- congenitally short cervix
- Uterine anomalies
- exposure to diethyl stilbesterol in-utero
- Previous instrumental delivery
- Previous precipitate labour
- Badly repair cervical laceration
- Excess and vigorous cervical dilatation.
- polymorphism in collagen 1A1 gene (COL1A1) and TGFB1 genes
- Pap smear procedure
CLINICAL PRESENTATION
- The abortion is usually painless and very rapid. It may be preceded by period of low back pain/pelvic heaviness.
- The abortion is usually preceded by passage of show and drainage of liquor.
- For each succeeding pregnancy, age of pregnancy reduce. In cases where the age of pregnancy is increasing of constant, think of uterine anomaly.
DIAGNOSIS
Diagnosis of cervical incompetence can be made by your doctor both in pregnancy and non-pregnancy state. Your doctor will take a detailed clinical history from you and carry out the following tests to make a definite diagnosis of cervical incompetence.
Non-pregnant state
- Hysterosalpingography: It is done during day 7-10 of menstrual cycle. There will be funneling of the cervical canal.
- Retrograde passage of hegar’s dilator; size 8 is diagnostic.
- Traction test: A pediatric catheter is passed into your uterine cavity and balloon is inflated with 1ml of fluid. A 600g weight is then attached to it. If the catheter is pulled out, there is cervical incompetence.
Pregnant state:
- Vagina examination: Gradual and painless dilatation of the cervix
- Serial ultrasound: Shows progressively increasing internal os diameter (Beaking sign)
- Internal os diameter >15mm in the first trimester
- Internal os diameter >20mm in the 2nd trimester
- Prolapsed of membrane through the cervical canal (bird beak sign)
- Shortened cervical length
- Cervical length measurement: A short cervical length is associated with cervical insufficiency. Cervical length <30mm as measured by transvaginal ultrasonoigraphy predicts preterm delivery with positive predictive value of 54% and negative predictive value of 95%. Should shortening and dilatation occurs, emergency or salvage cerclage is done but prophylactic cerclage is preferred at an early stage (14-16 week of gestation).
TREATMENT
- Cerclage pessary: This can be used instead of prophylactic cerclage but the efficiency of this has not been proven.
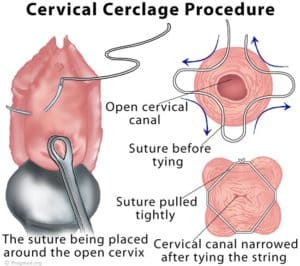
Image credit: www.pregmed.org
- Cervical cerclage procedure: The procedure There is no doubt that the name of Shirodkar will always be associated with this operation. However, in Western practice, the simpler McDonald suture, which is described here, is used, predominantly because of its simplicity. The operation is best planned when the patient is booked for delivery. It is usual to carry out the operation between 12 and 14 weeks of gestation. It is important to perform an ultrasound scan to Operations on the cervix 99 exclude fetal abnormality before embarking on the procedure. A variety of nonabsorbable sutures such as Prolene, Ethibond or Mersilene tape, can be used with a large needle. Monofilament sutures have the advantage of being easier to use, sliding through the cervical tissue with minimal trauma a d less risk of infection than the tape. The disadvantage is that they tend to cut into the cervix more, making them more difficult to remove.
Patient preparation
It is of value for the patient to have a stat dose of prophylactic antibiotics prior to surgery.
Anaesthesia
Either a light general anaesthetic or a spinal is ideal for carrying out this procedure.
The operation
Exposing and grasping of the cervix
The patient is placed in the lithotomy position and the cervix exposed by placing a Sims speculum in the vagina. The cervix is grasped using two or more sponge holders, one on the anterior and one on the posterior lip of the cervix. The cervix is gently drawn down, exposing the length of the cervix. By drawing the sponge holders first to one side and then the other, the lateral parts of the cervix can be easily reached with the needle.
Insertion of the suture
The McDonald suture is essentially a purse‐string suture. The suture is placed circumferentially around the upper body of the vaginal part of the cervix in four separate ‘bites’, starting either posteriorly or anteriorly based on the surgeon’s preference. To aid removal of the suture, it is advised to leave the threads about 4–5 cm long and create a knot before cutting the suture. This allows the thread to be hooked with a finger or instrument and the knot at the cervix cut. Placing the knot anteriorly makes it easier to remove in late pregnancy. Practice will determine the correct tension, which should be tight enough to just close the os but not so tight as to produce a pallor of the cervix.
Removal of the suture
Anaesthesia is not required. Removal must be performed before labour becomes established and is easily accomplished by exposing the cervix, grasping the long end of the suture as described above and cutting the suture at any of the points where it is visible on the exterior of the cervix and then by simply pulling the knot. The patient must be informed of the importance of early attendance at the hospital if there is a suggestion of labour beginning. Management is particularly difficult when the patient goes into premature labour and the decision to cut the suture or to leave it and possibly conserve the pregnancy has to be made. Potential complications include premature rupture of the membranes, chorioamnionitis, cervical rupture if the suture is not removed before the onset of labour and bleeding.
Post-operative management
- Bed rest for 24-48hours with the foot of the bed raised.
- Tocolysis e.g. salbutamol to prevent preterm contraction.
- Analgesic for pain.
- Antibiotics
- Counsel patient to avoid coitus.
References:
- A synopsis of obstetric and gynaecology: IFUMSA Synopsis Project, 2011.
- Bonney’s gynaecological surgery.
- Mayo Foundation for Medical Education and Research (MFMER)
- Video credit: www.EmpowHER.com

Dr. Adeyemo Olusola is a medical graduate of Olabisi Onabanjo University, Ogun State, Nigeria along with certificate in advanced diploma in Principles of Nutrition, Management and Leadership, Dublin and Certificate in Global Health from London School of Hygiene and Tropical Medicine. In addition to his numerous certifications, he is a certified Telemedicine Physician from Harvard Medical School, USA. He is an avid reader of books from different oases of life, expert in data analysis. “So many a time, I have seen people die avoidable death because of lack of knowledge or information, falling victim of fate. There is then a necessity laid on us to help arm our society to the teeth, as a healthy society cannot be detached from an informed one. Hence, there is need for healthgist.net. We hope you will have a wonderful stay on our website.”

