Until fibroid is symptomatic, it is really nothing to be worried about. Fibroid is a benign tumour (NOT CANCEROUS) of uterine smooth muscles. It is the most common tumour in women. It is present in one in four white women and in 80% of black women above the age of 25 years even if the size of seedling.
It is clinically detectable in about 20-30% of women over 30 years and can be classified into subgroups based on their relationship to the uterus:
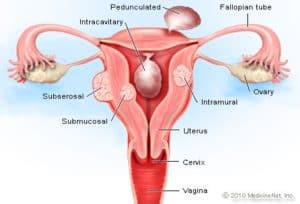
- Intra-mural: – Fibroid situated in the muscular wall of the uterus.
- Sub-serosa: – Fibroid situated just beneath the outermost layer of the uterus.
- Submucosa: – Fibroid situated just beneath the innermost (endometrium) layer of the uterus.
- Pedunculated fibroid: – It is connected to the uterus by a stalk.
RISK FACTORS (THINGS THAT COULD MAKE A WOMAN HAS FIBROID)
- Black race
- Positive family history
- Obesity
- Age above 25
- Nulliparity (a woman who has never carried pregnancy into age of viability- 24 weeks in UK but 28weeks in Nigeria).
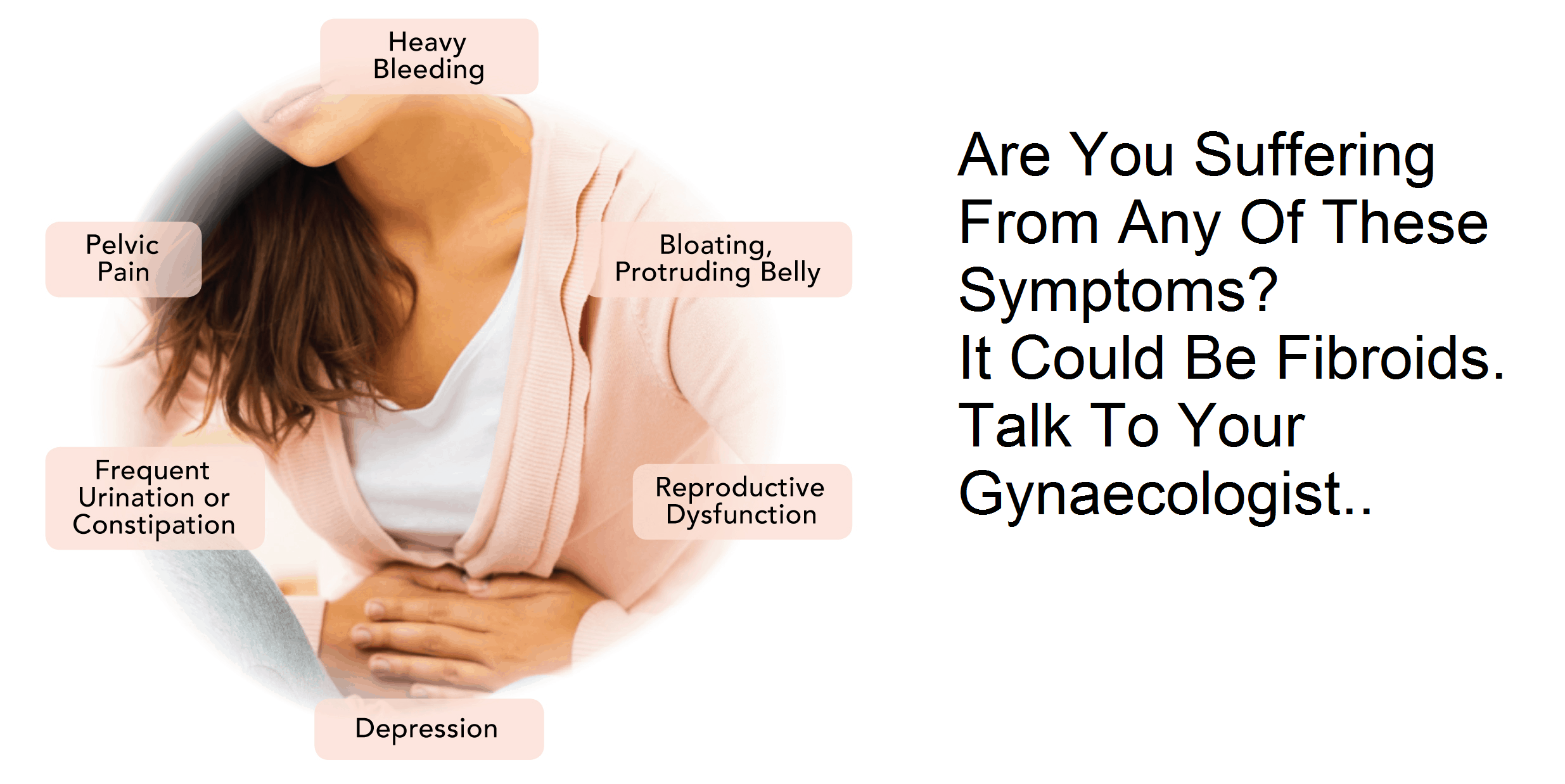
CLINICAL FEATURES
Unless fibroid becomes symptomatic, they do not require any treatment. This means that a woman can be asymptomatic (shows no symptoms).
Common presenting symptoms are:
- Heavy menstrual bleeding
- Iron deficiency anemia
- Pelvic pressure or pressure symptoms: – This may be a sense of progressive pelvic fullness, “something pressing down.” This is often caused by slowly enlarging fibroid. Pressure symptoms can present as:
- Urinary symptoms: – Frequency, retention etc
- Problem with defecation: – Constipation
- Lymphatic symptoms: – Oedematous leg swelling
- Abdominal pain
- Slowly progressive abdominal swelling
- Infertility: – This may result from mechanical distortion or occlusion of the fallopian tubes.
- Cases where there is pregnancy coexisting with fibroid, bleeding after delivery should be envisaged because of inefficient uterine contraction.
DIAGNOSIS (WHEN WILL YOUR DOCTOR SAY YOU HAVE FIBROID?)
Your doctor will make diagnosis of fibroid based on findings on physical examination and imaging studies.
On abdominopelvic examination, uterine fibroid usually present as a large midline, irregular-contoured mobile pelvic mass with a characteristic “hard feel” or “solid quality”. The degree of enlargement is usually stated in term (“weeks size”) that are used to estimate equivalent gestational size.
OPTIONS OF INVESTIGATIONS INCLUDE:
- Abdominal or Transvaginal ultrasonography: Either of these could in case of uterine fibroid reveal- Hypoechoic mass within the uterus, posterior shadowing from the mass, degenerating fibroids may have calcifications or cystic components, multiple fibroids appear as an enlarged, irregularly shaped, diffusely heterogeneous uterus. However, if cancerous, rapidly growing mass may be observed in the uterus.
- Hysterosalpingogram
- Abdominal x-ray
- Full blood count
- Electrolyte, urea and creatinine level
TREATMENT
There are two treatment options. This include medical and surgical. The essence of medical option is to help control bleeding, pain and shrink the tumour before surgery.
See HEAVY MENSTRUAL BLEEDING for treatment options in case of heavy menstrual bleeding.
If you are aneamic, your doctor will place you on iron supplement.
Gonadotropin-releasing hormone agonist (GnRH) is used to reduce fibroid size by as much as 40% to 60%. Examples of GnRH are gooserelin, buserelin, naferelin etc.
SURGICAL TREATMENT
- Myomectomy: – Your doctor will counsel you on myomectomy (removal of fibroid- see image below) as an option if you want to retain childbearing potential.

- Hysterectomy: – Your doctor will only consider this option if you have completed childbearing.
FURTHER READING
Gynaecology by Ten Teachers
A synopsis of Obstetric and Gynaecology
Beckmann and Ling’s Obstetrics and Gynaecology
IMAGE CREDIT: Google image

Dr. Adeyemo Olusola is a medical graduate of Olabisi Onabanjo University, Ogun State, Nigeria along with certificate in advanced diploma in Principles of Nutrition, Management and Leadership, Dublin and Certificate in Global Health from London School of Hygiene and Tropical Medicine. In addition to his numerous certifications, he is a certified Telemedicine Physician from Harvard Medical School, USA. He is an avid reader of books from different oases of life, expert in data analysis. “So many a time, I have seen people die avoidable death because of lack of knowledge or information, falling victim of fate. There is then a necessity laid on us to help arm our society to the teeth, as a healthy society cannot be detached from an informed one. Hence, there is need for healthgist.net. We hope you will have a wonderful stay on our website.”